The Common Vein Copyright 2010
Definition
Subacute thyroiditis or subacute granulomatous, de Quervains thyroiditis, is a self limiting inflammatory process of the thyroid gland. This condition is believed to be caused most often by viral infections, but reports of subacute thyroiditis have been linked to radiation therapy, paraneoplastic syndrome, and some medications.
Inflammation of the thyroid results in glandular destruction and dysfunction of the thyroid gland.
Structural changes include inflammatory cell infiltration, formation of multinucleated giant cells, and destruction of normal follicular glands.
Functional changes of subacute thyroiditis are related to the destruction of the glandular tissue. At first, destruction of colloid collections can lead to increased release of thyroid hormone, but eventually destruction of the tissue leads to decreased production.
Clinically, subacute thyroiditis most often presents 2-8 weeks after a viral illness with an enlarged painful thyroid gland. Fever, fatigue, malaise can also been seen during the acute phases of the disease. Patients may classically present with triphasic course of symptoms: hyperthyroidism followed by hypothyroidism and finally reaching a euthyroid state.
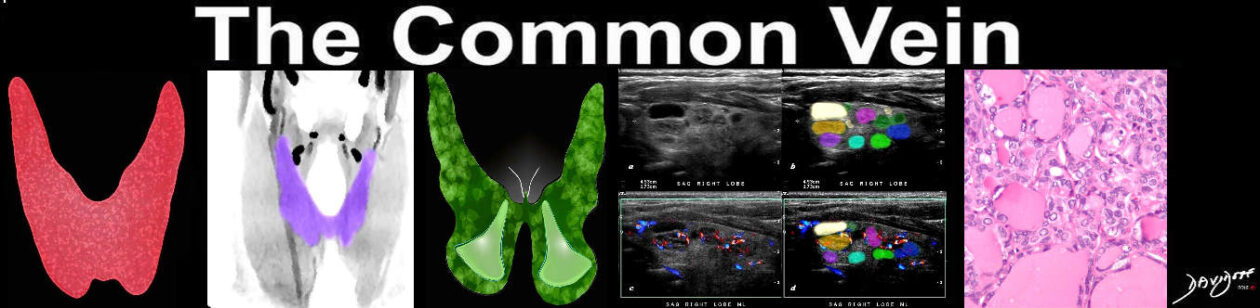
Imaging of subacute thyroiditis can be performed with ultrasound or thyroid scintigraphy. Ultrasound of the thyroid may reveal an enlarged hypoechoic thyroid gland with increased vascularity. Scintigraphy will show a low level of iodine uptake reflecting the decreased thyroid hormone synthesis. Diagnosis is best make clinically and can be confirmed with laboratory and imaging results.
Due to the self limiting nature of the disease, treatment is mainly symptomatic. NSAIDs and corticosteroids are highly effective in treating the pain and discomfort. beta blockers may be used to treat symptoms of hyperthyroidism.