Feedback Mechanisms
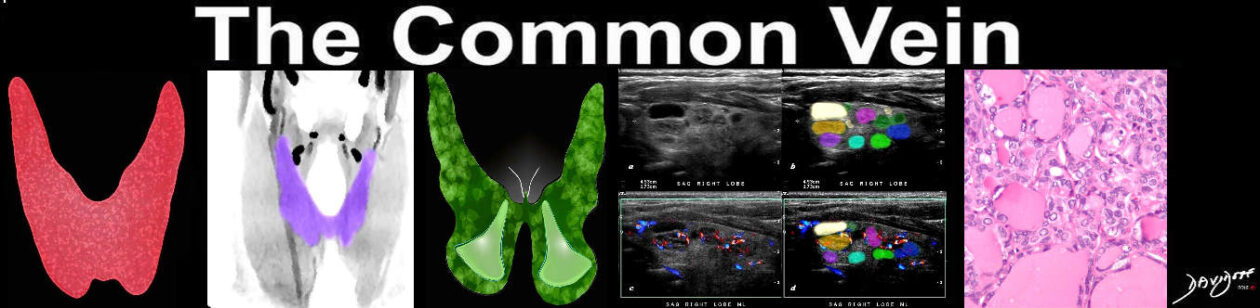
The Common Vein Copyright 2010
Basic Function of the Thryoid Axis and Feedback
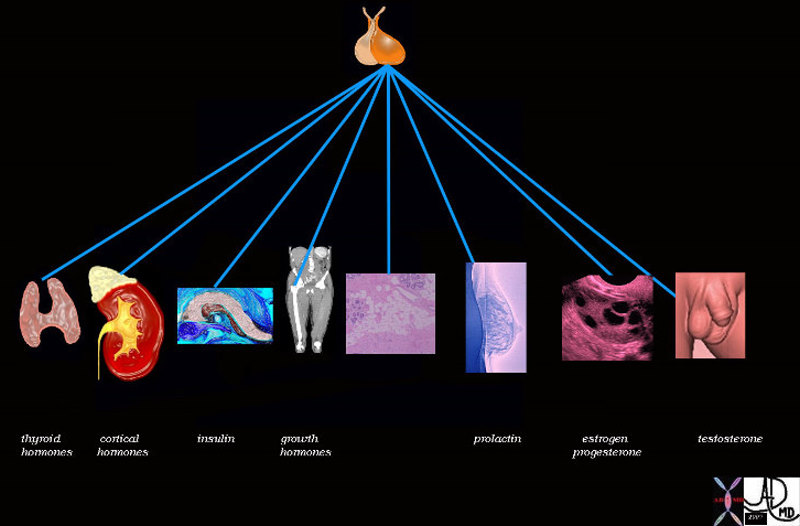
Pituitary Control |
|
The pituitary controls the function of the thyroid gland by the production of thyroid stimulating hormone (TSH). There is a reciprocal relationship between TSH and thyroid hormone levels. Image Courtesy Ashley Davidoff MD 72353 |
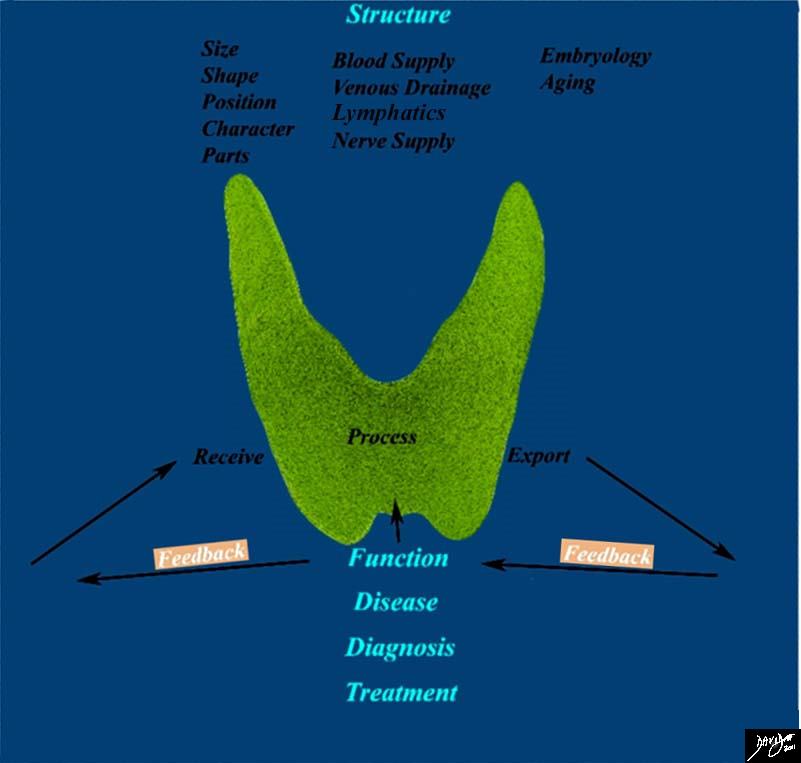
Feedback Mechanisms |
|
This diagram frames the underlying principles and approach to the thyroid in this module and focuses on the feedback function of the thyroid Image Courtesy Ashley Davidoff MD 93852g05.8sb04c |
TRH structurally is a tripeptide ((pyro)Glu-His-Pro-NH2) secreted from the hypothalamus, reaches the anterior pituitary gland through the portal system and its fuction is to stimulate TSH synthesis as well as subsequent release. Thyroid hormones give negative feedback inhibiting TRH production that’s why in Hypothroidism TRH production is raised. Since TRH also stimulates prolactin release from the pituitary is common to encounter hypothryroid women with hyperprolactinemia which can lead to galactorrhea, oligomenorrhea and/or amenorrhea.
TSH strucurally is a glycoprotein with 2 subunits: alfa (shared with other types of hormones) and beta (specific to bind thyroid gland receptors). Its main fuction is on the thyroid gland where stimulates receptors to promote thyroid gland proliferation and/or thyroid hormones release. TSH has the property to stimulates iodine trapping and biochemical transformation of T4, actually can stimulate T4 release within minutes.
TSH is release through out the day and night in a slow steady patern and its feedback is mainly related to circulating T3 in a negative manner.
T4 is the short name for levothyroxine, compound by four iodine atoms is consider as a prohormone, produced exclusively in the thyroid gland goes into the bloodstream and is converted by deiodination into T3, short name for triiodothyronine, that has three iodine atoms and is the active thyroid hormone being eight times more effective than T4. The convertion from T4 to T3 also occur inside the thyroid gland but in less quantity, although in cases of iodine deficiency or hyperthyroid states, the convertion in the thyroid gland increases and the actual ammount of T3 that is released from the thyroid gland raise. T4 highly bounds to proteins in the bloodstream while T3 is find mostly in its free form which allows to penetrate faster the target tissue or organ. As mention before thyroid hormones get produced by the direct stimulation of TSH and when they reach sufficient levels in plasma they inhibit or supress TSH production in the pituitary gland and TRH in the hypothalamic nuclei (supraoptic and supraventricular), stablishing a negative feedback, otherwise these two hormones are released continuosly resembling a circadian patern.
rT3 is an isomer of T3 and therefor can bind the thryoid hormone receptors but does not have the property to stimulate them, thereby blocks T3 action. It is produced by T4 deiodination and low quantities but becomes importan in certain pathological states like stress, where the adrenal glands increase the amount of cortisol in the blood, than cortisol inhibits the convertion of T4 to T3 leading to increase in the convertion of rT3, since this hormone is inactive the overall symptomatology will resemble hypothyroidism, this condition is called Reverse T3 Dominance.
Calcitonin structurally is a 32-amino acid linear polypeptide hormone produced by the thyroid gland and encharged of calcium regulation. Is produced in response to hypercalcemia with the purpose to shift calcium into the bone, however overall its effect in calcium regulation is not essential and that’s why after surgical removal of the thyroid gland there is no need to replace this hormone with supplemental medication.