The Common Vein Copyright 2010
Definition
Hyperthyroidism is an over production of thyroid hormones, thyroxine (T4) and triiodothyronine (T3) by the thyroid gland.
Hyperthyroidism can be caused by several different pathologies including Grave’s disease (the most common cause), toxic adenoma, toxic multinodular goiter, thyroiditis, and drugs.
Hyperthyroidism results in a clinical syndrome caused by increased levels of metabolically active free T3 and T4 in the bloodstream. Symptoms typically include tachycardia, agitation, tremors, hyperreflexia, heat intolerance and weight loss. The clinical syndrome of hyperthyroidism, when pronounced, is called thyrotoxicosis.
At its most dangerous, elevated thyroid hormone concentration can cause thyroid storm which is a medical emergency accompanied by a fever and change in mental status.
Structural changes of hyperthyroidism depend on the underlying cause, but include diffuse hypertrophy of the entire gland (as in Graves’ disease) or a single hyperactive toxic nodule.
Functional changes define the disease and consist of increased production of thyroid hormones despite negative feedback.
Clinically, patients will present with thyrotoxicosis, a large constellation of symptoms which include tremor, weight loss, insomnia, heat intolerance and irritability.
Imaging modalities to diagnose hyperthyroidism mainly include thyroid ultrasound and thyroid scintigraphy. Ultrasound can be used to distinguish between multinodular goiter, single nodule, and diffuse hypertrophy. Thyroid scintigraphy with radioiodine tracer uptake can show either localized increased uptake, such as in a “hot” or toxic nodule, or diffuse increased uptake, as in Grave’s disease.
Although imaging is available, diagnosis is best made with laboratory tests showing both a decreased TSH level and an increased circulating level of T3 and T4.
Treatment depends on the cause of hyperthyroidism, but includes medications that inhibit thyroid hormone production (methimazole and PTU), and medications that block the increased metabolic effect of the hormones, such as beta blockers. Some cases are best treated with radioisotope (Iodine-131) ablation of the gland. Surgical thyroidectomy is the least common treatment.
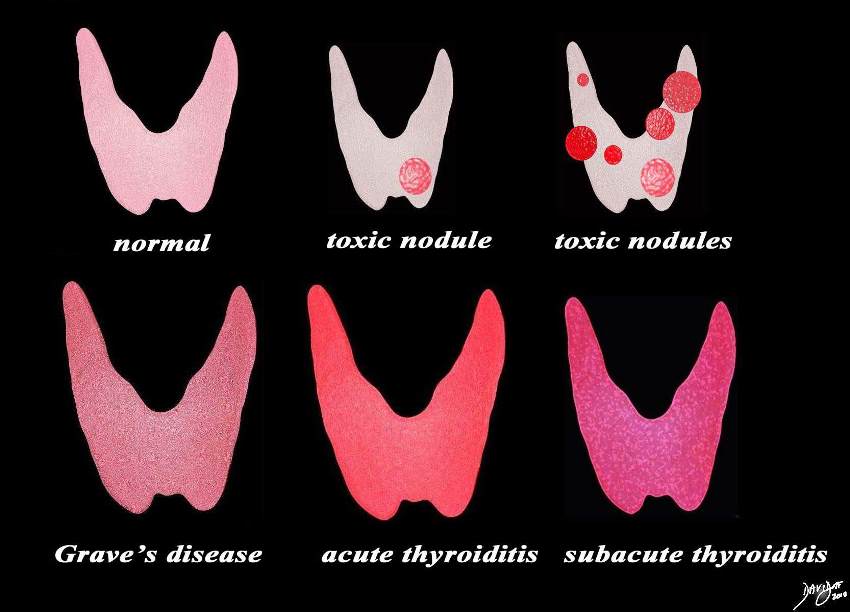
The Structural Faces of Hyperthyroidism |
|
This diagram shows rtthe structural possibilities in a patient who presents with thyrotoxicosis. Reading from upper left the normal thyroid is shown for reference of size and normal activity (pink). Next is the single toxic nodule that suppresses the function of the gland and the also causes the rest of the gland to shrink. This is followed by a diagram of multiple toxic nodules and the gland in this case may also be smaller than normal. The lower series of images include Grave’s disease, which is the most common cause of thyrotoxicosis, followed by acute thyroiditis and then subacute thyroiditis. Courtesy Ashley Davidoff MD copyright 2010 all rights reserved 93852.d03cdc06.8s |
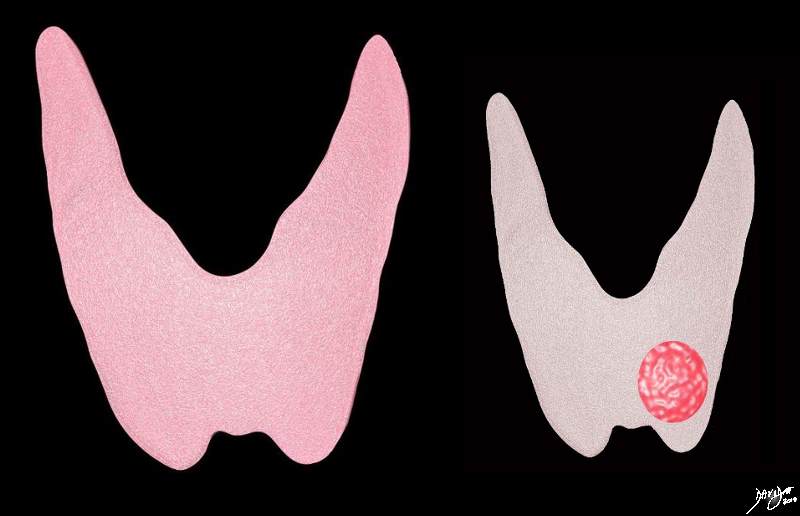
Normal Thyroid and Gland with Toxic Nodule |
|
The diagram outlines a normal gland on the left (pink) and an abnormal gland with a toxic hypefunctioning nodule in the left lobe (red). As a result of its hyperfunction it supresses the rest of the gland which becomes atrophied. The color gray reflects this lack of function. Courtesy Ashley Davidoff MD copyright 2010 all rights reserved 93852.d.8d.8s |
Thyrotoxicosis is a hypermetabolic state where there is a serum elevation of the thyroid hormone levels, essentially free T4 and T3, meaning thyroid hormone excess. Thyrotoxicosis is the syndrome resulting from tissues being exposed to significantly elevated levels of thyroid hormone; most casese are due to hyperthyroidism, namely excessive thyroid gland activity. One significant example of thyrotoxicosis not being caused by hyperthyroidism is the ingestion of excessive exogenous thyroid hormone. The most common cause of hyperthyroidism caused by a thyroid disorder is Graves’ disease; toxic MNG and toxic adenomas are others.
Structural changes define the etiology of the disease; in this sense autoimmune disease causes Graves’ disease. Lymphocytic thyroiditis and postpartum thyrotoxicosis result from increased release of thyroid hormones due to inflammation. Intrinsic thyroid tissue developing as a neoplasm can cause hyperproduction of thyroid hormones by autonomic hyperproduction leading to a toxic state; an example is a solitary toxic nodule or toxic adenoma, as well as multinodular goiter. Very rare but also possible is an infectious cause of thyrotoxicosis like subacute thyroiditis or acute suppurative thyroiditis, where an abscess results in destruction of thyroid tissue due to bacterial infiltration. Release of excess thyroid hormones results. Thyrotoxic states can also develop caused by excessive exogenous thyroid hormone ingestion or iodine load. Certain drugs like amiodarone have a known effect in thyroid function causing either hyperthyroidism or destructive thyroiditis, as well as hypothyroidism in some patients.
Clinical manifestations or hyperthyroidism include: weight loss despite an often increased appetite, insomnia, palpitations and tachycardia, fatigue and weakness, tremors, anxiety, shortness of breath, diarrhea or increase number of bowel movements, irregular menses, flow murmur, heat intolerance with warm moist skin, and hyperreflexia with rapid phase of relaxation.
Diagnosis includes a very thorough history and physical examination a long with laboratory data and imaging studies. Laboratory studies begin with TSH. It is suppressed in hyperthryoidism. Elevated free T4 and free T3 may help ocnfirm the diagnosis and its degree. The classic scenario for thyrotoxicosis is a primary etiology of the thyroid gland that leads to a complete suppressed TSH level with high-normal to frankly elevated T4 and T3 levels. It is also important to obtain complete blood count, basic metabolic panel and liver profile because these can be affected secondarily by increased thyroid hormone action. When thyrotoxicosis is caused by Graves disease TSH receptor antibodies TSI and TBII are usually detectable, as well as antithyroid peroxidase and antithyroglobulin antibody. It is usually not necessary, however, to measure these titers. The diagnosis of Graves disease is usually clear from exam and imaging studies.
Imaging studies help to differentiate between hyperthyroid states, which is very important because the type of treatment will rely on diagnosis. Thyroid ultrasound is used primarily for structural information, specifically with question of thyroid nodules. It helps to visualize and discriminate single or multipel nodules. Color-flow Doppler may aid by characterizing flow patterns, as flow is often high in toxic nodules and low mainly seen in thyroiditis or exogenous thyroid exposure. Another advantage of using US is that can be used in breastfeeding women who cannot be exposed to radioactive iodine.
Thyroid scans help to differentiate etiology in thyrotoxicosis functionally by radionuclide administration (123I, I131 or technetium Tc 99). In cases of hyperthyroidism caused by Graves’disease the thyroid scan will reveal diffuse increased radionulide uptake. For nodules with autonomous hyperfunction, radionuclide uptake is prominent in a solitary focus, or increased in multiple spots within the thyroid gland with toxic multinodular goiter. Most often when a radioactive iodine scan test is performed, an uptake of tracer at 24 hours is measured as well. Uptake measures the amount of radioactive material taken up by the thyroid gland, and is inappropriately high in hyperthyroid states and inappropriately low in thyroiditis and with exogenous hormone intake.
All the adrenergic symptoms of hyperthryoidism, regardless of etiology, can be treated with beta-blocker therapy. Other options of treatment will depend on the primary diagnosis. For Graves disease, toxic multinodular goiter and toxic adenomatreatment usually begins with antithyroidal drugs. Radioactive iodine (131I) and thyroid surgery are more definitive treatments. Thyroiditis is often treated with steroids as part of the first line treatment, effectively countering the inflammation involved.