Assistant
Introduction
The primary function of the thyroid is to produce and secrete the metabolic hormones thyroxine and triiodothyronine, as directed by control pathways within the endocrine system. This process may be broken down into four sections: Receiving, Processing, Export, and Control.
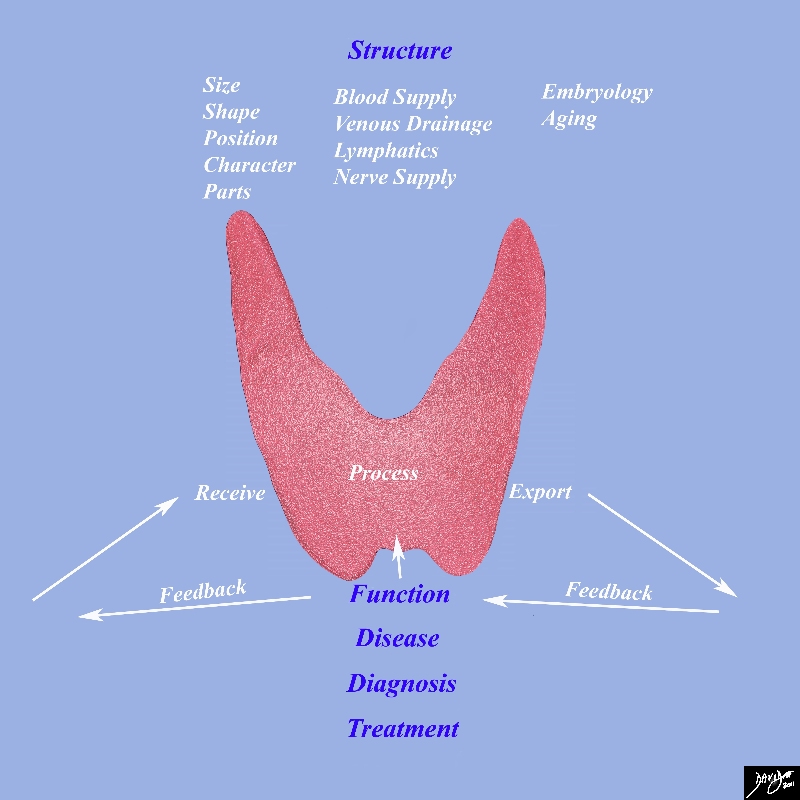
Thyroid Function receiving Processing Exporting and Feedback Mechanisms Under Master Control of the Pituitary |
|
This diagram frames the underlying principles and approach to the thyroidin this module This diagram frames the underlying principles and approach to the thyroid in this module Since the thyroid is a biological structure its morphological characteristics are defined by its size, shape position and character. As a biological unit it needs to be connected with other structures and it does this via blood vessels lymphatics and nerves. It functions with the basic notion that it receives processes and exports its product. All structures whether they are the smallest cell to the largest organ work in the same way. They receive process and export their product. Biological structures are subject to disease which may affect structure and or function. We use diagnostic methods to identify aberrant structure and or function and we apply therapeutic regimens to correct aberrant structure and function Image Courtesy Ashley Davidoff MD 93852g05c.8s |
Receiving
Synthesis of the thyroid hormones thyroxine and triiodothyronine requires a steady supply of iodine, a chemical element found in nature and supplied by diet in most developed countries. The average adult must consume 50 mg of iodine per year to maintain proper thyroid function. Approximately four fifths of that ingested iodine is excreted by the kidneys, but the remaining one fifth, ~10 mg per year, is selectively gathered by thyroid cells and used to produce mass quantities of thyroxine and triiodothyronine.
This process, commonly referred to as iodine trapping, occurs through the action of a large number of iodide pumps located in the basal membrane of each follicular epithelial cell. In response to endocrine activation these pumps transport free iodide from the bloodstream to the interior of the cell, concentrating it to a level up to 250 times that found in the blood.
Processing
Once inside the cell this free iodide sequentially binds to tyrosine sites in thyroglobulin, a glycoprotein produced by follicular epithelial cells, in a process called organification. As a result of this sequential iodination approximately 30 molecules of thyroxine and 3 molecules of triiodothyronine are synthesized within every molecule of thyroglobulin.
Hormone-laden thyroglobulin is then secreted with colloid into the follicles where it is stored until required by the body for metabolic activation. Owing to the thyroid’s large number of follicles, the thyroid is able to store enough hormone to supply the body with normal levels of thyroxine and triiodothyronine for two to three months.
Exporting
When the supply of thyroxine and triiodothyronine in the blood becomes depleted a cascade of endocrine signaling is initiated that induces the pinocytotic uptake of colloid and thyroglobulin by follicular epithelial cells. Inside the cell thyroglobulin is digested by a series of enzymes, simultaneously releasing thyroid hormone and cleaving iodine to be reused for further hormone synthesis. Thyroxine and triiodothyronine, now freed, diffuse through the base of the thyroid cell and into the surrounding capillaries where they are transported to tissues throughout the body.
Control
Regulation of the synthesis and secretion of thyroid hormone occurs through a negative feedback inhibition pathway in the endocrine system. When the concentration of thyroxine and triiodothyronine in the blood dips below a certain level thyrotropin-releasing hormone (TRH) is released from the hypothalamus, resulting in subsequent release of thyroid stimulating hormone (TSH) from the anterior pituitary gland. Receptors on the base of each follicular epithelial cell bind to TSH, activating intracellular cAMP pathways that initiate a series of stimulatory effects in each thyroid cell. These effects include the increased proteolysis of thyroglobulin to release thyroxine and triiodothyronine, increased activity of iodine pumps, increased iodination of tyrosine, increased size and secretory activity of existing thyroid cells, and proliferation of new thyroid cells. While proteolysis of thyroglobulin occurs almost immediately, the majority of TSH’s effects require days or weeks to occur, resulting in a well-choreographed effort to increase and stabilize basal metabolic rate. Once the thyroid’s rate of secretion increases to 1.75 times its normal rate thyroid hormone acts directly on the anterior pituitary gland to inhibit further secretion of TSH. As a result, thyroid secretion gradually decreases and the concentration of thyroxine and triiodothyronine in the blood is kept constant.
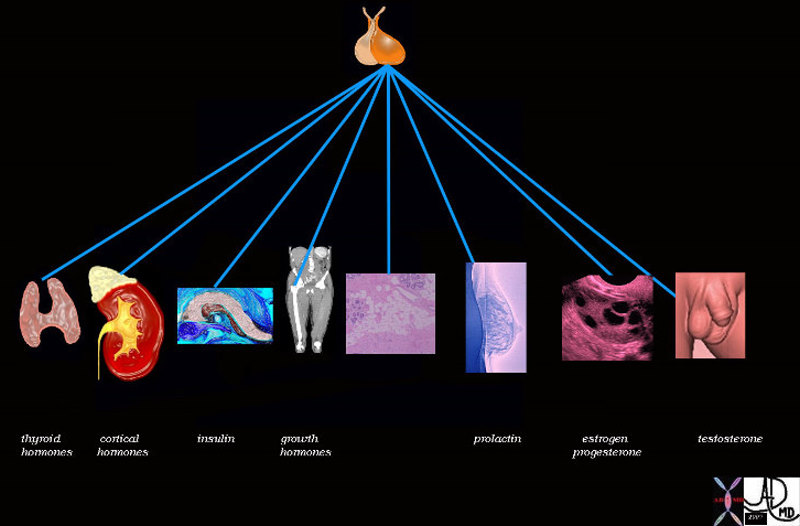
Pituitary Gland – Master Control of the Endocrine System |
| 72353 pituitary gland posterior pituitary gland thyroid adrenal cortex pancreas insulin bone muscle growth adipose tissue fat glucose parathyroid gland calcium breast lactation prolactin ovary estrogen FSH progesterone testis testes testosterone function physiology specialised function control endocrine system Davidoff art Davidoff drawing Davidoff MD |