Thyroid Volume 19 Number 11 2009
Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL,Mandel SJ, Mazzaferri EL, McIver B, Pacini F, Schlumberger M, Sherman SI, Steward DL, Tuttle RM.
ABSTRACT
BACKGROUND:
Thyroid nodules are a common clinical problem, and differentiated thyroid cancer is becoming increasingly prevalent. Since the publication of the American Thyroid Association’s guidelines for the management of these disorders was published in 2006, a large amount of new information has become available, prompting a revision of the guidelines.
METHODS:
Relevant articles through December 2008 were reviewed by the task force and categorized by topic and level of evidence according to a modified schema used by the United States Preventative Services Task Force.
RESULTS:
The revised guidelines for the management of thyroid nodules include recommendations regarding initial evaluation, clinical and ultrasound criteria for fine-needle aspiration biopsy, interpretation of fine-needle aspiration biopsy results, and management of benign thyroid nodules. Recommendations regarding the initial management of thyroid cancer include those relating to optimal surgical management, radioiodine remnant ablation, and suppression therapy using levothyroxine. Recommendations related to long-term management of differentiated thyroid cancer include those related to surveillance for recurrent disease using ultrasound and serum thyroglobulin as well as those related to management of recurrent and metastatic disease.
CONCLUSIONS:
We created evidence-based recommendations in response to our appointment as an independent task force by the American Thyroid Association to assist in the clinical management of patients with thyroid nodules and differentiated thyroid cancer. They represent, in our opinion, contemporary optimal care for patients with these disorders.
Section Text
FULL ARTICLE ATA GUIDELINES PDF file
Introduction
What you need to know
Follicles are normal
Macrofollicles are normal
Microfollicles are not normal
Nodules in 7-10 % of Population by Palpation
Incidence By Ultrasound (40-50% – >60%)
50 year old 50% have nodule/s
60 year old 60% have nodule/s
70 year old 70% have nodule/s
Of all nodules 95% will be benign
Of all malignant lesions 75-85% will be papillary carcinoma which is usually an indolent disease.
Thus small % of malignant tumors have bad prognosis
Papillary carcinoma has increase 3 fold since 1988
Papillary Carcinoma (75-85%)
Follicular Carcinoma (10-20%)
Medullary Carcinoma (5%)
Anaplastic Carcinoma (<3%)
Other – squamous type, lymphoma
What is the appropriate evaluation of clinically or incidentally discovered thyroid nodule(s)?
What laboratory tests and imaging modalities are indicated?
What is the role of fine-needle aspiration (FNA)?
What is the best method of long-term follow up of patients with thyroid nodules?
How should thyroid nodules in children and pregnant patients be managed?
Size and Nodules
“Generally, only nodules >1 cm should be evaluated, since they have a greater potential to be clinically significant cancers. Occasionally, there may be nodules <1 cm that require evaluation because of suspicious US findings, associated
lymphadenopathy, a history of head and neck irradiation, or a history of thyroid cancer in one or more first-degree relatives. However, some nodules <1 cm lack these warning signs yet eventually cause morbidity and mortality. These are rare and, given unfavorable cost/benefit considerations, attempts to diagnose and treat all small thyroid cancers in an effort to prevent these rare outcomes would likely cause more harm than good”
Deteremine History for increased risk eg radiation in childhood family history (Cowden’s Carney Complex MEN 2 Werner)
Examine for fixation and cervical adenopathy
Serum TSH and US scan
TSH low ie thyroxine is high ie hyperthyroid – NM scan
TSH high ie thyroxine is low ie hypothyroidism – associated with increased risk of malignancy
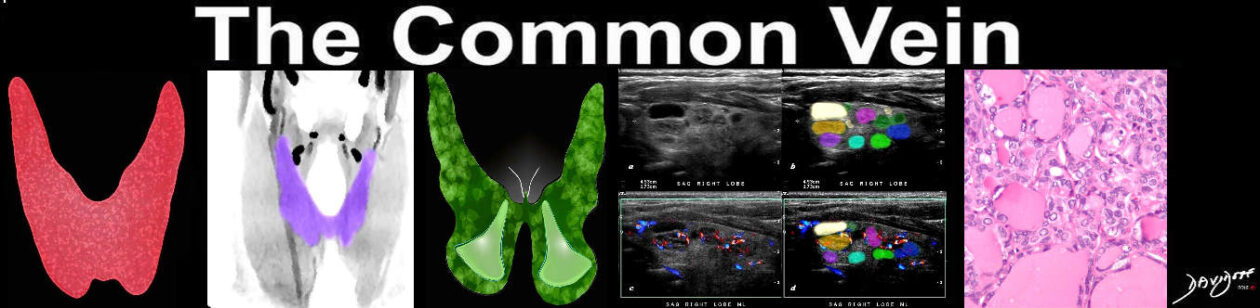
“Diagnostic thyroid US should be performed in all patients with a suspected thyroid nodule, nodular goiter, or radiographic abnormality; e.g., a nodule found incidentally on computed tomography (CT) or magnetic resonance imaging ( MRI) or thyroidal uptake on 18 FDG-PET scan.”
microcalcifications (papillary)
hypoechogenicity (papillary) iso or hyper (follicular
irregular margins
irregular halo
absent halo
cigar shape
central hypervascularity
Pure cystic
Colloid –
spongiform appearance
Hot nodules have a negligible association with cancer
“Approximately 1–2% of people undergoing 2- deoxy-2[18F]fluoro-d-glucose positron emission tomography
(18 FDG-PET) imaging for other reasons have thyroid nodules discovered incidentally. Since the risk of malignancy in these
18 FDG-positive nodules is about 33% and the cancers may be more aggressive (20), such lesions require prompt evaluation
(21–23). When seen, diffuse 18 FDG uptake is likely related to underlying autoimmune thyroiditis.”
nondiagnostic,
suspect benign
follicular lesion of undetermined significance (risk of malignancy 5–10%).
indeterminate or (neoplasm, either follicular or Hurthle cell
neoplasm’’ (risk of malignancy 15–25%)
suspicious for malignancy (risk of malignancy 50–75%)
malignant (risk of malignancy at surgery >95%),
It is recommended that all benign thyroid nodules be followed with serial US examinations 6–18 months.after the initial FNA. If no growth then follow up 3-5 years
There is no consensus on the definition of nodule growth, however, or the threshold that would require rebiopsy. One reasonable definition of growth is a 20% increase in nodule diameter with a minimum increase in two or more dimensions of at least 2 mm. If growth is demonstrated – repeat biopsy ()remebere – measure solid portion of cystic lesions)
References
Hoang J, Kit, W Lee, M, et al US features of Tyhyroid Malignancy Pearls and Pitfalls RadioGraphics, 27,847-860.