The Common Vein Copyright 2010
Definition
Papillary carcinoma is a primary malignant neoplasm of the thyroid gland. It is the most common primary cancer of the thyroid gland. Papillary carcinoma is caused by radiation induced or sporadic genetic mutations resulting in malignant transformation.
Structural changes include formation of an asymptomatic firm mass or nodule. There are typically no functional changes of the thyroid gland.
Clinically, patients often are completely asymptomatic. Some patients may present with a palpable thyroid mass, while others with more advanced disease may have symptoms of dysphagia, vocal cord dysfunction, or pain. Upon presentation, 10-15% of patients will have distant metastases.
Imaging of papillary carcinoma includes ultrasound, thyroid scintigraphy, and CT. Ultrasound can characterize nodules as solid, cystic or complex. There are also several sonographic features of a thyroid nodule that are more suspicious for papillary carcinoma such as calcifications, irregular borders, and/or hypoechogenicity. On thyroid scinitgraphy, most papillary carcinomas will be “cold” nodules without much iodine uptake. CT can show local tissue invasion, suspicious lymph node involvement, and/or distant metastases. Although imaging can give good insight into the diagnosis of papillary carcinoma, fine needle aspiration biopsy is the gold standard and best way to diagnose thyroid papillary carcinoma.
Treatment of papillary carcinoma includes surgery, radioactive iodine, and/or chemotherapy. Patients may undergo thyroid lobectomy, subtotal or total thyroidectomy depending on the size and aggressive nature of the carcinoma. Radioactive Iodine can be used to treat remaining tissue or metastases. In many cases, patients will need permanent thyroid hormone replacement.
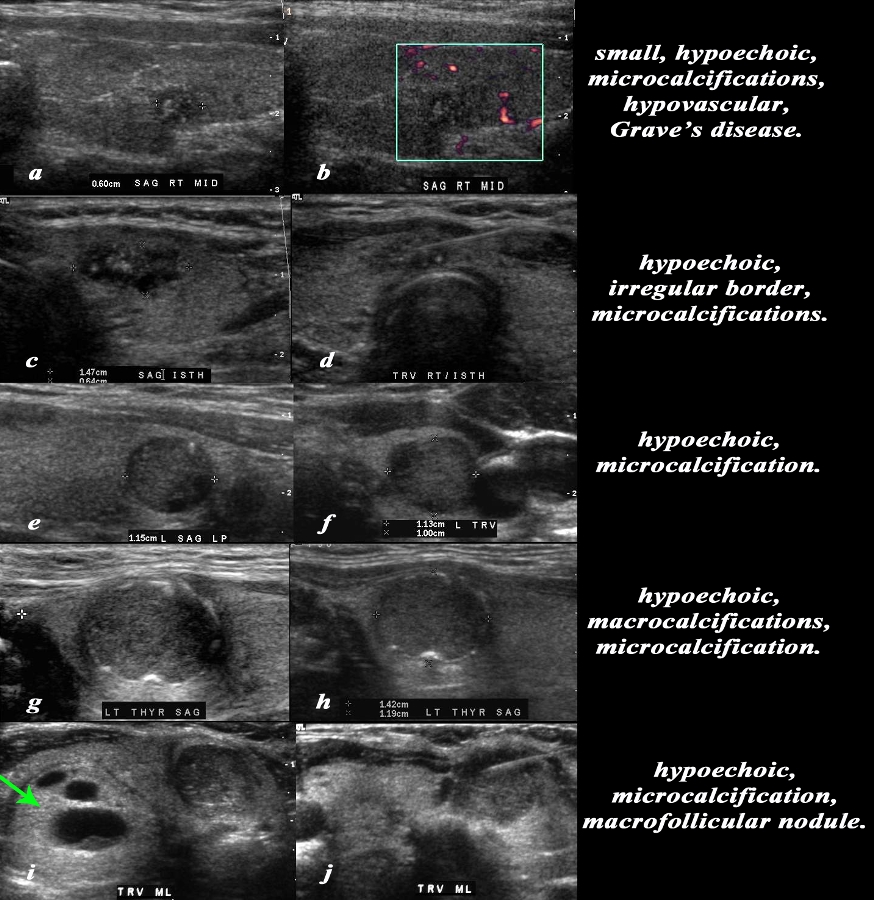
Variations in Ultrasound Findings |
|
This series reveals a range of findings on ultrasound in patients with papillary carcinoma. The first patient (a,b) is a female with Grave’s disease who reveals a 6mm nodule which is hypoechoic, hypovascular with microcalcifications. The second patient (c,d) is a 34 year old female patient who demonstrates a 1.5cms hypoechoic lesion with microcalcifications. Image c shows the biopsy needle in the lesion which is in the isthmus. The third patient (e and f) is a female patient with a well defined mildly hypoechoic nodule that has a single microcalcification in e. The fourth patient (g,h) is a 30 year old female who demonstrates a well defined, 1.4cms, mildly hypoechoic lesion with macroscopic shadowing calcification and a suggestion of microcalcification as well. The fifth patient (i,j) is a female patient with a hypoechoic lesion to the left of midline with microcalcification seen in (i), with biopsy needle noted in the lesion in (j), and a mixed macro/microfollicular lesion to the right of midline (green arrow in i). Courtesy Barry Sacks MD Copyright 2010 97067c.8 |
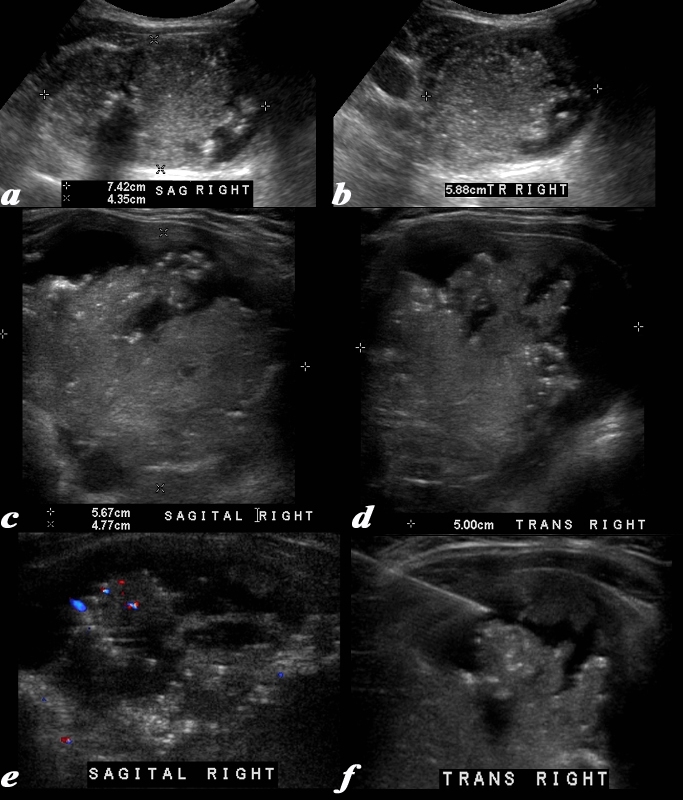
Microcalcifications Hypovascularity – Papillary Carcinoma |
|
This 63 year old male presents with an enlarged thyroid Ultrasound shows a mass in the right lobe of the thyroid. The right lobe measures 7.4cms in sagittal (a), 4.4 cms in A-P dimension (a) and 5.9cms in transverse view A complex mass is noted in the right lobe. with innumerable small echogenic foci consistent with non shadowing microcalcifications. High resolution imaging of the mass using a linear transducer shows the mass to consist of fronds of tissueand the microcalcifications nare better visualized. The mass measures 5.7cms in sagittal (c) and 5 cms in transverse view (d). Doppler study shows hypovascularity (e) and image f shows a biopsy needle in close proximity to the microcalcifications. A diagnosis of papillary carcinoma was made based on the biopsy Courtesy Ashley Davidoff MD Copyright 2010 96145c.8L |
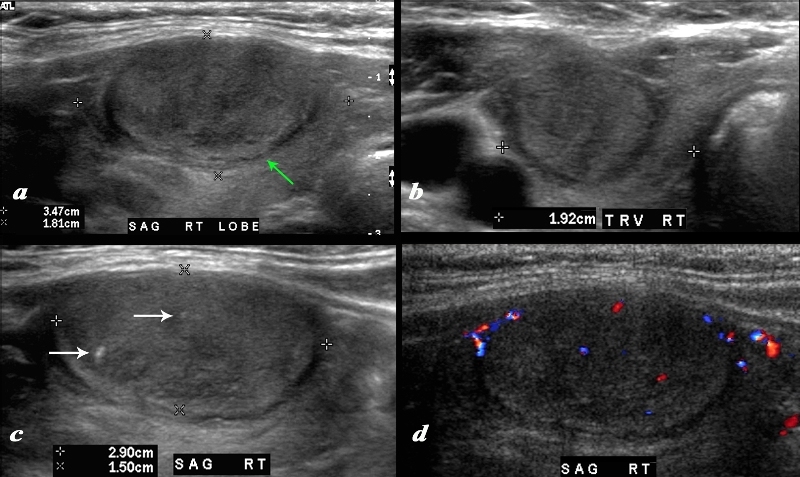
Large Papillary Carcinoma |
|
A large nodule in the thyroid occupies almost the entire right lobe (a). The nodule measures 2.9cms by 1.5cms. The gland is not enlarged and measures 3.5cms (craniocaudad), by 1.8cms (A-P) by 2.4cms (transverse). The nodule is almost isoechoic with normal thyroid but shows internal irregular areas of hypoechogenicity, regions of isoechogenicity, as well as microcalcifications (white arrows (c). There is irregularity of the border at the posterior aspect of the nodule green arrow a). The halo shows irregular borders in this region as well. Internal vascularity is minimal (d). The irregular surface is concerning for a malignant processes. The diagnosis in this patient was papillary carcinoma Courtesy Ashley Davidoff MD Copyright 2010 74909c02L.8 |
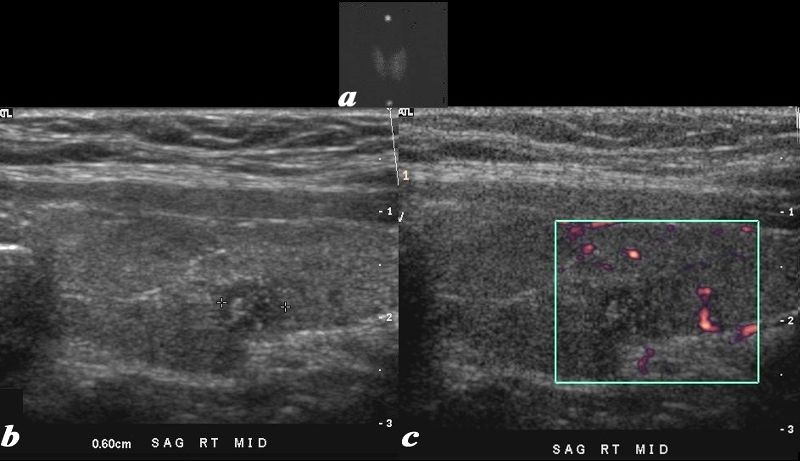
Papillary Carcinoma and Grave’s Disease |
|
This series includes a nuclear medicine thyroid scan, and an ultrasound of a patient with Grave’s disease and a small papillary carcinoma. Image(a), is a rather small nuclear medicine thyroid scan and shows diffuse increase in uptake of the radioisotope in a enlarged gland confirming the underlying clinical apparent graves disease. Image b is a sagittal view of the right lobe of the thyroid and shows a 6mm hypoechoic solid lesion with microcalcifications. Image c shows hypovascularity of the lesion. A biopsy was performed and papillary thyroid carcinoma in a patient with Graves’s disease was diagnosed. Courtesy Barry Sacks MD Copyright 2010 97025cL.8 |
|
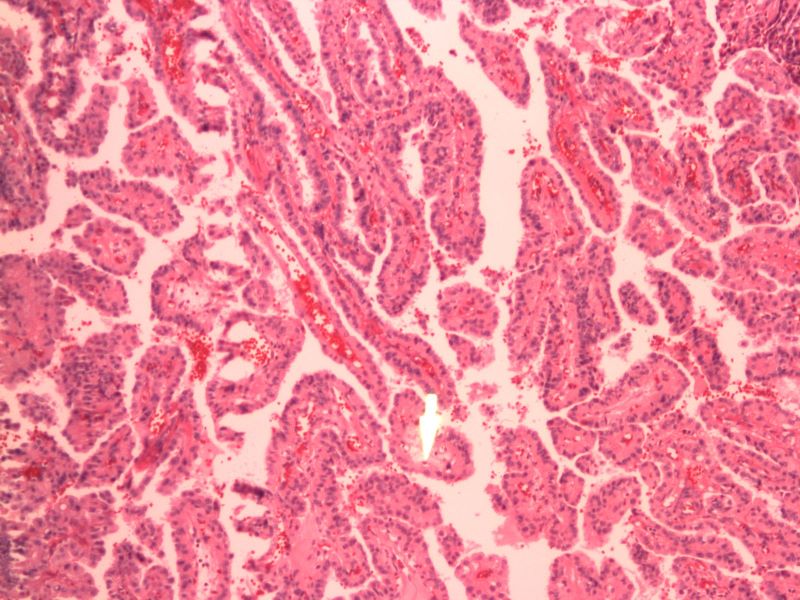
Finger-Like Shape 10X H&E |
|
The histological section at 10X magnification using H&E stain shows a papillary carcinoma with papillary architecture. Papillary means a “nipple” but papillary morphology means that the shape of the tumor is reminiscent of finger like projections. Image Courtesy Ashraf Khan MD. Department of Pathology, University of Massachusetts Medical School. 99414.8 |
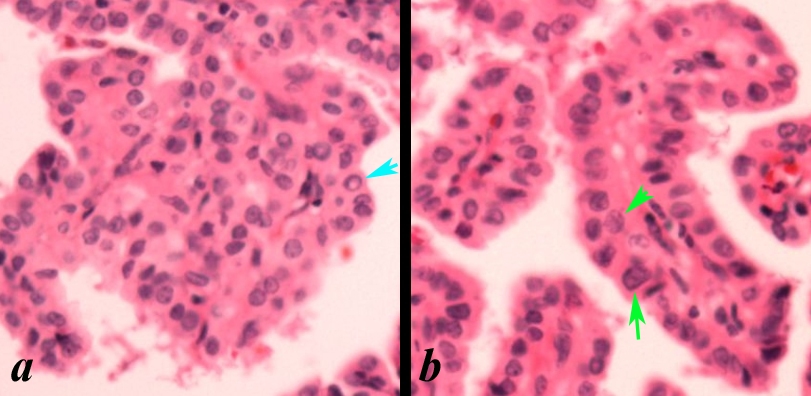
Orphan Annie Eyes and Nuclear Grooves |
|
This high power view (>20X) shows papillary cancer nuclei with Orphan Annie nuclei and grooves. Orphan Annie nuclei a “cleared-out” or empty appearance, similar to Little Orphan Annie’s eyes (light blue arrow in a). Nuclear grooves characteristic lines that run across the nuclei (green arrows in b). Image Courtesy Ashraf Khan MD. Department of Pathology, University of Massachusetts Medical School 99413c01 |
|
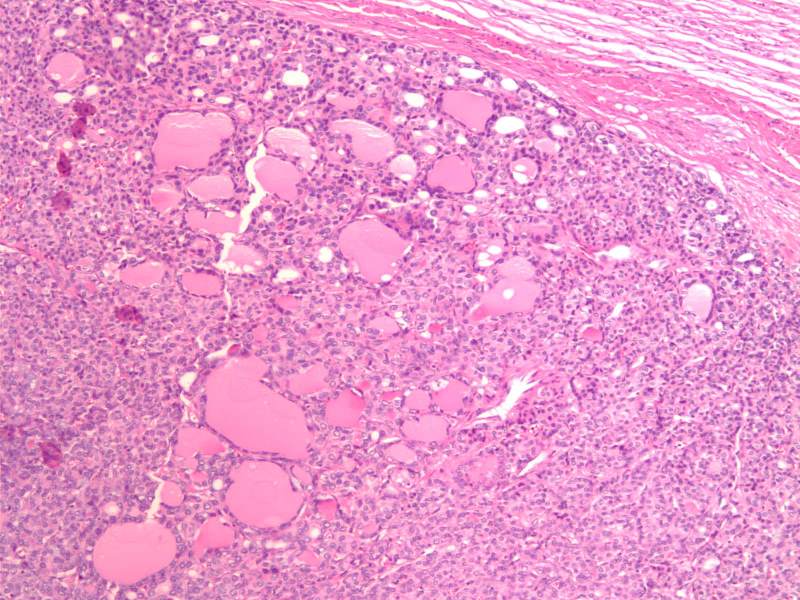
Encapsulated Follicular Variant of Papillary Carcinoma |
|
The histological section at 10X magnification using H&E stain shows a encapsulated follicular variant of papillary carcinoma (FVPC) with microfollicular architecture. Image Courtesy Ashraf Khan MD. Department of Pathology, University of Massachusetts Medical School. 99397.8 |
|
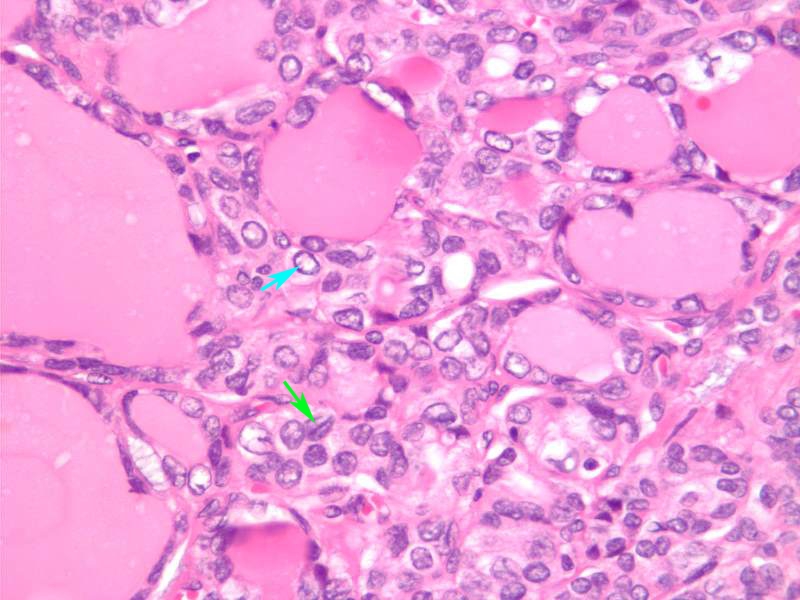
Encapsulated Follicular Variant of Papillary Carcinoma 40X H&E |
|
The histological section at 40X magnification using H&E stain shows a encapsulated follicular variant of papillary carcinoma (FVPC) with microfollicular architecture. This high power view shows papillary cancer nuclei with Orphan Annie nuclei and grooves. Orphan Annie nuclei a “cleared-out” or empty appearance, similar to Little Orphan Annie’s eyes (light blue arrow). Nuclear grooves characteristic lines that run across the nuclei (green arrow). Image Courtesy Ashraf Khan MD. Department of Pathology, University of Massachusetts Medical School. 99398.81 |