Barry Sacks MD Ashley Davidoff MD
The Common vein Copyright 2010
Introduction
Clinical problem and Statistics
Nodules in 7-10 % of Population by Palpation
Incidence Much Higher By Ultrasound (40-50% – >60%)
Of all nodules 95% will be benign
Of all malignant lesions 95% will be papillary carcinoma which is usually an indolent disease.
Thus small % of malignant tumors have bad prognosis
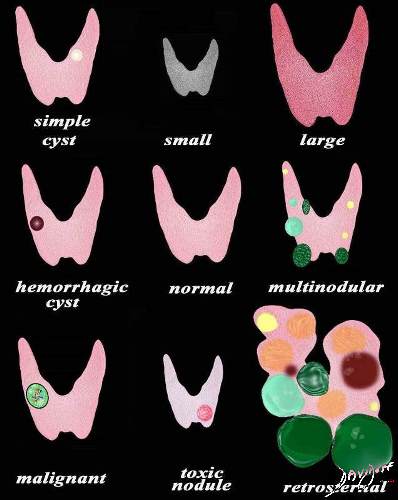
The diagram illustrates a range of nodules that can affect the thyroid. Based on thyroid function tests and sometimes with the aid of a nuclear scan the nodules are divided into functioning or non-functioning. If they are hyperfunctioning they are called “toxic” (bright red nodules) and if not then they are called “non-toxic”. When they are hyperfunctioning they suppress the function of the normal thyroid and hence the normal thyroid in these cases are grayed out. Morphologically they may be single or multiple, large or small. When they cause thyroid enlargement they are called a goiter. From a pathological perspective nodules may be benign or malignant. The benign nodules have a wide ranges of microscopic findings. The primary malignant lesions include follicular carcinoma, papillary carcinoma and medullary carcinoma.
Courtesy Ashley Davidoff MD Copyright 2010 93852e07h01a04L.8s
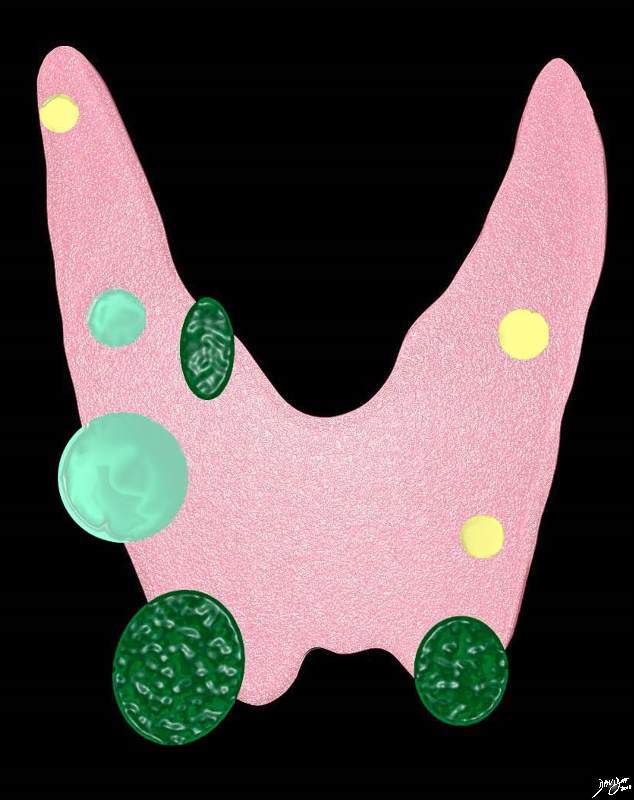
The multinodular goiter in this diagram is a combination of simple cysts (yellow), complex cysts (light green) and solid nodules (dark green). Characterisation of complex and solid lesions is best first evaluated by
Courtesy Ashley Davidoff MD copyright 2010 all rights reserved 93852.d13.8s
AdenomaPathology
Macrofollicular adenoma (simple colloid)
Microfollicular adenoma (fetal)
Embryonal adenoma (trabecular)
Hürthle cell adenoma (oxyphilic, oncocytic)
Atypical adenoma
Adenoma with papillae
Signet-ring adenoma
Carcinoma
Papillary (75 percent)
Follicular (10 percent)
Medullary (5 to 10 percent)
Anaplastic (5 percent)
Other
Thyroid lymphoma (5 percent)
Cyst
Simple cyst
Cystic/solid tumors (hemorrhagic, necrotic)
Colloid Nodule
Dominant nodule in a multinodular goiter
Other
Inflammatory thyroid disorders
Subacute thyroiditis
Chronic lymphocytic thyroiditis
Granulomatous disease
Developmental abnormalities
Dermoid
Rare unilateral lobe agenesis
Challenge Is Which Require Workup
Criteria for the Imaging and Follow-up of Thyroid Nodules
Clinical
Age And Sex Of Patient
>1-1.5 Cm
Single Vs Multiple
Firm To Palpation
Family History
Radiation Exposure
Imaging Considerations
Ultrasound very good at extremes
Macrofollicular and mixed macro/micro on one extreme
Obvious neoplasms especially papillary carcinoma on the other
heterogenous lesions usually indeterminate
Should biopsy the most hypoechoic region
Should biopsy all hypoechoic lesions even < 1cm, especially when margins irregular
Microcalcifications with comet tail or ring down less concerning
Other microcalcifications more concerning
Benign features
Larger Nodules More Often Benign
Smooth Round or Oval
Texture similar to normal thyroid
Homogeneous lesion
Cystic Changes
Hypoechoic thin halo
Vascular Pattern Usually hypovascualr and peripheral – though papillary are hypovascular
Peripheral egg shell calcification
Malignant features
Malignancies Can Be Small
Irregular shape
Hypoechoic or heterogeneous
Not usually cystic
Irregular margins
thick halo or irregular halo
Microcalcifications
Extremely Vascular
Calcification
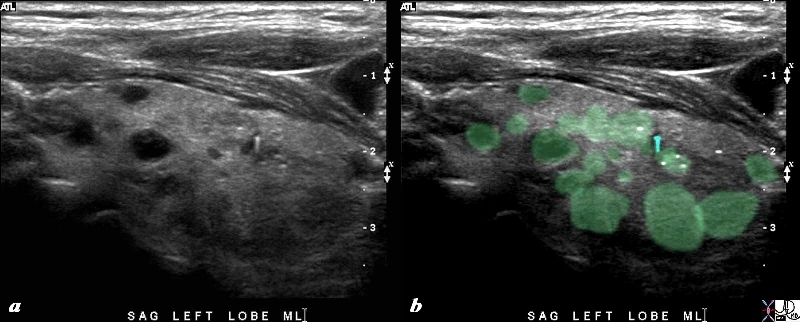
The 80 year old male presents with an asymptomatic multinodular goiter, consisting many nodules of varying size and echogenicity.
A microcalcification with ring down artifact is seen overlaid in teal blue. Other microcalcifications are probably present (overlaid in white). The multiple nodules that are not border forming are within the confines of the parenchyma and do not alter the shape of the gland. The right lobe of the thyroid measures about 4.5 cms in sagittal 1.5cms.in A-P dimension, and 1.5cms in the transverse plane. The gland is therefore not enlarged These findings are consistent with a non toxic multinodular thyroid gland, and not truly a goiter since the gland is not enlarged. The ringdown or comet tail artifact characteristic of small calcifications is exemplified in this image and is usually a sign of benign calcification. On the other hand the fine echogenicities without ring down artifact are more concerning.
Courtesy Ashley Davidoff MD Copyright 2010 94780c06L.8s
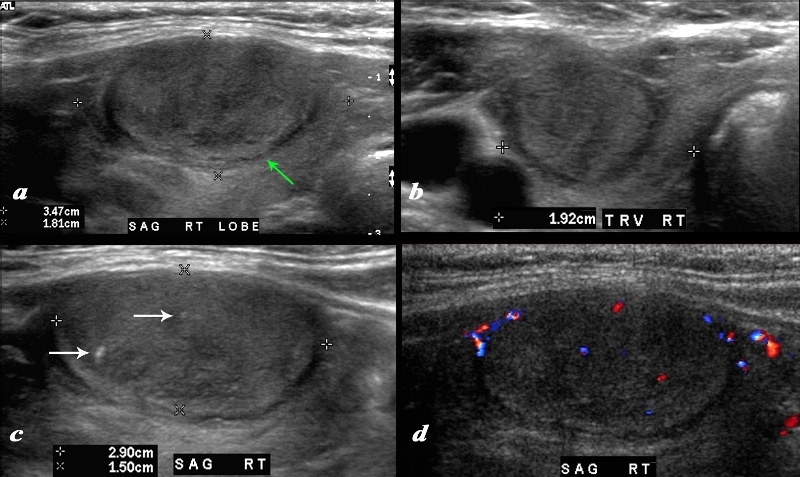
Large Irregular Halo, Microcalcifications
A large nodule in the thyroid occupies almost the entire right lobe (a). The nodule measures 2.9cms by 1.5cms. The gland is not enlarged and measures 3.5cms (craniocaudad), by 1.8cms (A-P) by 2.4cms (transverse). The nodule is almost isoechoic with normal thyroid but shows internal irregular areas of hypoechogenicity, regions of isoechogenicity, as well as microcalcifications (white arrows (c). There is irregularity of the border at the posterior aspect of the nodule green arrow a). The halo shows irregular borders in this region as well. Internal vascularity is minimal (d). The irregular surface is concerning for a malignant processes. The diagnosis in this patient was papillary carcinoma
Courtesy Ashley Davidoff MD Copyright 2010 74909c02L.8
Biopsy from the opposite side
Technique
Medial to lateral
25g needles – no aspiration Use capillary vacuum of the 25gauge needle
4 passes into different regions
smear slides and immediately fix
inject remainder into cytolyte
if ? Lymphoma – send flow cytometry
Features to be evaluated by ultrasound
Overall gland size for each lobe
Sagital images for length and depth
Transverse image for width
Nodules
for nodules > 1.0 cm and any other suspicious nodules
Measure three dimensions (sagital and transverse images)
Assess colour flow and record image
Primary features of malignancy for nodules
Microcalcifiction
Macrocalcification
Solid Nodule
Image to assess cystic areas and mural nodules
Colour flow central
Greater than surrounding thyroid
Features suggestive of benignancy
Cystic nodules
Peripheral (eggshell) calcification
Soft findings
Peripheral calcification – benign
Taller than wide – malignant
Profoundly hypoechoic < muscle – malignant
Which nodules to image
All nodules > 1 cm except for multinodular gland with diffuse similar nodules
Any smaller nodules noted to be highly suspicious for malignancy
Solid, microcalcifications, internal colour flow
When to recommend FNA
Microcalcification
If > 1.0 cm or smaller nodules if also solid and/or internal colour flow
Mainly solid or macrocalcification
If > 1.5 cm
Not purely cystic (no mural nodule)
If > 2.0 cm
Substantial interval growth
When to recommend follow up
None of the above
Multinodular gland with diffuse bilateral similar nodules (little visible normal thyroid tissue)
Multiple nodules
Biopsy the largest or most suspicious 2 or 3 nodules > 1.0 cm
Timing of follow up
follow up at 6 months then 12, 24 and 36 months.
References
Frates Mary C Benson C.B et al Management of Thyroid Nodules Detected at US: Society of Radiologists in Ultrasound Consensus Conference Statement
Radiology, 237, 794-800. December 2005
Norman J MD endocrineweb Fine Needle Biopsy of Thyroid Nodules
Robert T. Pu M.D., Ph.D., Jack Yang M.D., Patricia G. Wasserman M.D., Tawfiqul Bhuiya M.D., Kent A. Griffith M.P.H., M.S., Claire W. Michael M.D. Does Hurthle cell lesion/neoplasm predict malignancy more than follicular lesion/neoplasm on thyroid fine-needle aspiration? Diagnostic Cytopathology Vol 34 Issue 5 pages 330-4 May 2006
Consensus Panel 2004
Welker M.D Mary Jo., Orlov, Diane M.S., C.N.P. Thyroid Nodules American Family Physician Feb 2003