The Common Vein Copyright 2010
Definition
Hashimoto’s thyroiditis is an autoimmune disorder that leads to antibody mediated destruction of thyroid gland.
The most common causative antibodies responsible for Hashimotos thyroiditis are anti- thyroid peroxidase (anti-TPO), anti-thyroglobulin (anti-Tg), and anti-TSH receptors.
The immune destruction of the thyroid follicular cells results in glandular destruction and hypothyroidism.
Structural histopathologic changes of Hashimoto’s include lymphocytic cell infiltration, fibrotic change, and formation of lymphoid follicles that replace the normal glandular tissue. Structural changes can range from an enlarged goiter to atrophy of the thyroid gland.
Clinically, patients suffering from the disease may have transiently increased thyroid hormone release during initial destruction of the thyroid follicles, but in general the disease is characterized by a hypothyroid state with a non-functioning thyroid gland. Classically, hashimoto’s will present with insidious onset of hypothyroidism progressing over months to years. These symptoms include fatigue, constipation, weight gain, cold intolerance, menstrual irregularities.
Imaging is not particularly useful for the diagnosis, but sonographic features of Hashimoto’s thyroiditis are evident and suggestive. Radioactive iodine scans may show a generalized decreased iodine uptake at later stages of the disease.
Treatment for Hashimoto’s thyroiditis is based on thyroid hormone replacement, most often with levothyroxine (synthetic T4).
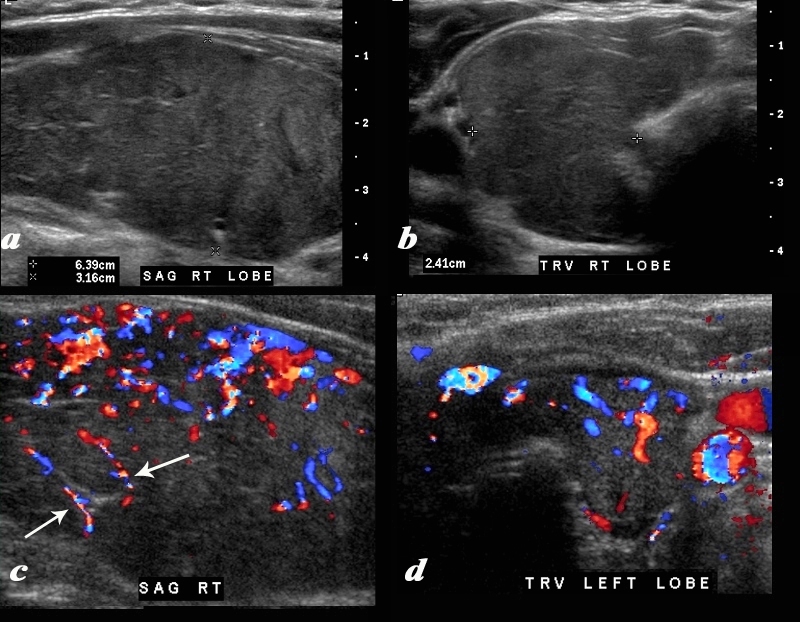
Enlargement Fibrous Strands and Hypervascularity |
|
A diffusely enlarged, heterogeneous thyroid gland is seen in this 30 year old hypothyroid female patient. The thyroid measures 6.4cms (craniocaudad), by 3.2cms (A-P) by 2.4cms (transverse). Clinical findings were consistent with thyroiditis, with biochemical findings suggesting hypothyroidism. The sagittal view shows coarse heterogeneous echo texture with fine white bands consistent with fibrosis. The increased vascularity is seen throughout the gland (c,d), but is also seen particularly along some of the bands in the posterior aspect of the gland (c arrows). The enlarged gland in the transverse dimension is almost round. (b). This rounded shape in the transverse dimension is a clue to the presence of the enlarged gland, even before the measurements are taken and evaluated. The findings are consistent with a thyroiditis. Courtesy Ashley Davidoff MD Copyright 2010 94583c01.8 |
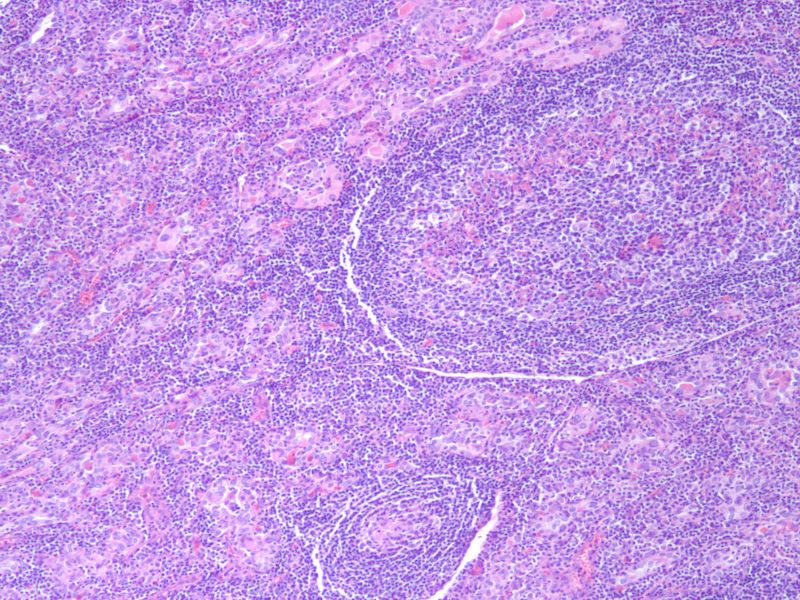
Hashimoto’s Thyroiditis – Atrophic Follicles Lymphocytic Infiltrate 10X H&E |
|
The histological section at 10X magnification using H&E stain shows atrophic follicles with Hurthle cell change and dense lymphocytic infiltrate in the stroma Image Courtesy Ashraf Khan MD. Department of Pathology, University of Massachusetts Medical School. 99401.8 |
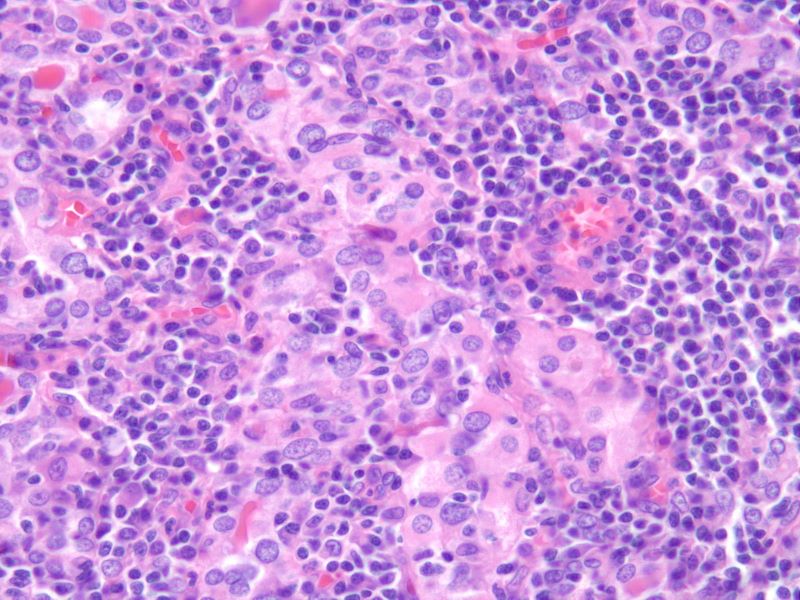
Hashimoto’s Thyroiditis – Atrophic Follicles, Hurthle Cells, Lymphocytic Infiltrate 40X H&E |
|
The histological section at 40X magnification using H&E stain shows atrophic follicles with Hurthle cell change and dense lymphocytic infiltrate in the stroma Image Courtesy Ashraf Khan MD. Department of Pathology, University of Massachusetts Medical School. 99402.8 |